Move Freely, Live Fully – Advanced Shoulder Care for Lasting Pain Relief and Mobility!
Move Freely, Live Fully – Advanced Shoulder Care for Lasting Pain Relief and Mobility!
Shoulder pain shouldn’t hold you back. Dr. Apoorv Dua offers advanced treatments to restore strength, flexibility, and comfort for conditions such as:
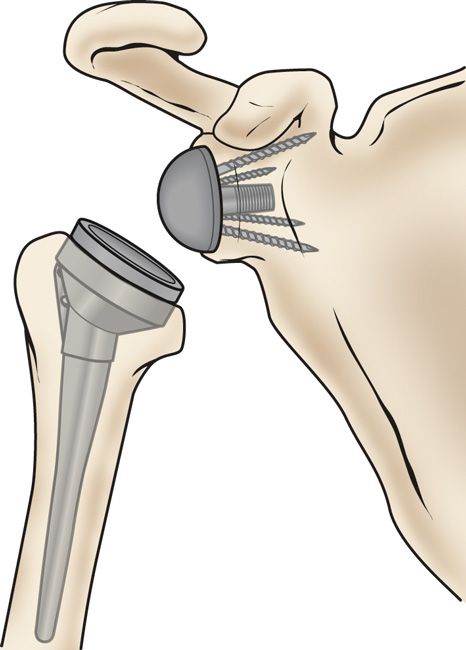
Shoulder replacement, also known as shoulder arthroplasty, involves removing damaged bone and replacing it with metal and plastic implants.
The shoulder is a ball-and-socket joint, where the round head of the upper arm bone fits into a shallow socket. Damage to this joint can cause pain, stiffness, and weakness.
Implants come in various shapes and sizes, with options including partial or total replacement, using either anatomic or reverse designs.
Shoulder replacement surgery is highly successful, with most patients experiencing significant pain relief and improved mobility. Overall satisfaction rates are around 90%.
About Shoulder Replacement
 Symptoms
Symptoms
 Diagnosis
Diagnosis
 How We Perform
How We Perform
 Why Is Treatment Needed?
Why Is Treatment Needed?
 Recovery
Recovery
 Rehabilitation
Rehabilitation
 Prevention
Prevention
Shoulder replacement surgery is performed to relieve pain and restore function in a damaged shoulder joint.
Common conditions leading to shoulder joint damage include:
Osteoarthritis: Wear-and-tear arthritis that damages cartilage, affecting smooth joint movement.
Rotator cuff injuries: Damage to the muscles and tendons surrounding the shoulder can also harm cartilage and bone.
Fractures: Breaks in the upper arm bone (humerus) may necessitate replacement, especially if prior fracture repair fails.
Rheumatoid arthritis and other inflammatory disorders: Chronic inflammation can damage cartilage and sometimes the underlying bone.
Osteonecrosis: Reduced blood flow to the humerus can cause bone collapse, affecting joint integrity.
A doctor evaluates whether shoulder replacement surgery is needed through a combination of physical examination and imaging/tests:
Physical Exam: Checks for visible changes in the shoulder, assesses pain levels at rest and during movement, and evaluates range of motion and strength.
X-rays: Show joint space narrowing or bone changes to confirm arthritis.
CT Scan: Provides detailed images of bone structure and integrity.
MRI: Assesses soft tissues, including the rotator cuff tendons and cartilage.
EMG or Nerve Conduction Study: Ordered if nerve damage is suspected, to evaluate nerve function.
Shoulder replacement surgery involves replacing the damaged ball-and-socket joint with a prosthetic. The procedure typically follows these steps:
Anesthesia: The patient is given general or regional anesthesia for comfort and pain control.
Incision: A surgical cut is made to access the shoulder joint.
Removal of Damaged Parts: The damaged ball (humeral head) and/or socket (glenoid) are removed.
Insertion of Prosthetic Parts: Artificial components made of metal, plastic, or ceramic are implanted to restore joint function.
Closure: The incision is closed with sutures or staples, and the shoulder is dressed and bandaged.
Shoulder replacement is a surgical procedure that replaces a damaged shoulder joint with a prosthetic to relieve pain and restore function. It is usually recommended when non-surgical treatments fail, and the patient continues to experience significant pain or limited mobility.
Common reasons for shoulder replacement include:
Arthritis: Wear-and-tear or inflammatory arthritis damaging the joint cartilage.
Shoulder instability: Recurrent dislocations or joint instability causing pain and dysfunction.
Severe pain: Persistent pain that limits daily activities despite conservative treatment.
Previous injuries: Fractures or injuries that have damaged the joint.
Avascular necrosis: Loss of blood supply to the humeral head leading to bone collapse.
Recovery after shoulder replacement varies by individual but generally takes 3 to 6 months for full recovery.
Key Points:
Pain and swelling: Expect discomfort and swelling to decrease within the first few days.
Physical therapy: Begins within 1–2 weeks to strengthen shoulder muscles and improve range of motion.
Activity restrictions: Avoid heavy lifting, sudden movements, reaching overhead, putting your arm behind your back, or using it to push yourself up.
Blood thinners: Follow your doctor’s instructions carefully if you are on blood-thinning medication.
Pain management: Take pain medication as prescribed by your doctor to ensure comfort and aid recovery.
Rehabilitation aims to restore shoulder function through structured physical therapy, focusing on improving strength, flexibility, and stability. Gradually, functional activities are reintroduced to help you return to daily life with better shoulder health.
Key Points:
Customized exercises to restore strength and range of motion.
Targeted movements to enhance shoulder flexibility.
Strengthening routines to rebuild stability and support.
Pain management techniques and medications as needed.
Gradual return to daily tasks and activities.
Preventing shoulder injuries involves strengthening the muscles, using proper techniques during activities, and avoiding overuse. Warm-ups, stretching, and ergonomic adjustments help maintain proper alignment and reduce the risk of injury.
Key Points:
Strengthen shoulder muscles to support joint stability.
Use correct techniques during sports and physical activities.
Avoid repetitive strain and overuse of the shoulder.
Warm-up and stretch before engaging in intense activities.
Maintain proper posture and alignment during daily tasks.
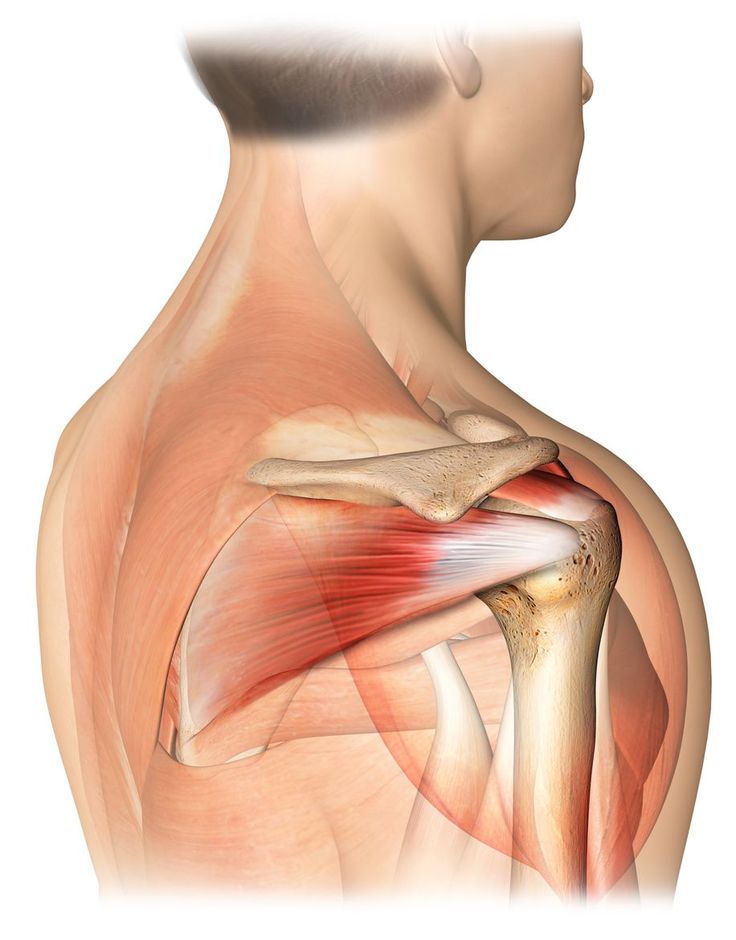
The rotator cuff is a group of muscles and tendons that stabilize the shoulder joint, allowing you to lift and rotate your arm. It is essential for everyday movements and overall shoulder function.
Causes of Rotator Cuff Injury:
Sudden trauma, such as falling on an outstretched hand.
Repetitive overhead or strenuous activities over time.
Degeneration due to aging, which weakens the tendons.
Rotator Cuff Repair Surgery:
If non-surgical treatments don’t relieve pain or restore function, surgery may be necessary. This can include:
Removing bone spurs that pinch the shoulder.
Repairing torn tendons or muscles.
Reattaching the tendon to the head of the humerus.
Surgical Techniques:
Arthroscopy: Minimally invasive surgery using small incisions and a camera.
Open Surgery: Traditional method with a larger incision.
Combination: Using both approaches when needed.
Goal of Surgery:
Restore shoulder function and flexibility.
Relieve pain not controlled by conservative treatments.
Improve strength and stability for daily activities.
About Rotator Cuff Repair
 Symptoms
Symptoms
 Diagnosis
Diagnosis
 How We Perform
How We Perform
 Why Is Treatment Needed?
Why Is Treatment Needed?
 Recovery
Recovery
 Rehabilitation
Rehabilitation
 Prevention
Prevention
Rotator cuff injuries are common, especially among athletes, construction workers, or anyone performing repetitive overhead or strenuous shoulder movements. Injuries can also result from falls or direct trauma to the shoulder.
Symptoms of a Rotator Cuff Injury:
Pain in the shoulder when lifting, lowering, or rotating the arm.
Pain that worsens at night or when resting the arm.
A dull, persistent ache in the shoulder.
Weakness in the shoulder, making it difficult to lift or rotate the arm.
Popping, clicking, or crackling sensations during movement.
Limited range of motion in the shoulder.
Pain severe enough to prevent sleeping on the affected side.
Sharp or stabbing sensations in the shoulder during certain movements.
These symptoms can affect daily activities and, if persistent, may require medical evaluation for diagnosis and treatment.
Physical Examination:
The healthcare provider will palpate (press on) different areas of the shoulder to locate tenderness or abnormalities.
Your arm will be moved into various positions to assess pain, flexibility, and range of motion.
Muscle strength around the shoulder and arms will be tested to identify weakness or functional deficits.
Imaging Tests:
X-rays: While rotator cuff tears themselves don’t appear on X-rays, these images can reveal bone spurs, arthritis, or other structural issues contributing to pain.
Ultrasound: Uses sound waves to visualize muscles, tendons, and other soft tissues. It allows dynamic assessment, meaning the shoulder can be examined during movement, and provides comparison with the healthy shoulder.
MRI (Magnetic Resonance Imaging): Offers detailed images of all shoulder structures, including muscles, tendons, and cartilage, providing a comprehensive view to confirm a tear or other injury.
These diagnostic steps help the doctor determine the severity of the injury and guide appropriate treatment.
Rotator cuff repair surgery is performed to reattach torn rotator cuff tendons to the upper arm bone (humerus). The procedure can be done using one of two main approaches:
1. Arthroscopic Repair
A small camera called an arthroscope is inserted through a tiny incision in the shoulder.
The surgeon uses the live images from the camera to guide instruments through additional small incisions to repair the torn tendon.
This minimally invasive method usually allows for outpatient treatment, meaning you can often go home the same day.
2. Open Repair
A larger incision is made to access and repair the tendon directly.
This approach is used for larger or more complex tears, or if arthroscopy is not feasible.
Both methods aim to restore shoulder function, reduce pain, and improve mobility. Recovery and rehabilitation plans may vary depending on the technique and severity of the tear.
Rotator cuff repair surgery is designed to restore shoulder function, improve flexibility, and relieve pain. Your doctor may recommend surgery if any of the following apply:
Persistent shoulder pain or weakness that hasn’t improved with other treatments.
A large tear in the rotator cuff (greater than 3 cm).
Symptoms that have lasted 6 to 12 months without improvement.
High activity levels, especially involving overhead work or sports.
A recent, acute injury causing significant tendon damage.
Failure of conservative treatments, such as at least two months of physical therapy, to relieve symptoms.
Surgery aims to repair the damaged tendon, improve strength, and allow a return to normal activities.
Recovery after rotator cuff repair depends on the size of the tear and individual healing factors:
Healing time: Tendons generally heal to the bone within about 6 weeks, but full tendon recovery can take up to 9 months.
Return to activities: Most daily activities can usually be resumed after approximately 12 weeks. Vigorous sports or heavy lifting may be restricted for 4–6 months.
Shoulder strength: Full recovery of shoulder muscle strength may take up to 9 months.
Pain: Some pain or soreness is normal for several months after surgery and should gradually improve over time.
Rehabilitation and physical therapy play a crucial role in regaining strength, flexibility, and function during this period.
Rehabilitation after rotator cuff repair is essential to restore shoulder function, strength, and flexibility. The process is carefully structured and often guided by a physical therapist to ensure optimal recovery.
Key Components:
Tailored exercises: Personalized programs help regain strength and improve mobility.
Range of motion movements: Specific exercises restore flexibility and prevent stiffness.
Strength training: Focuses on rebuilding shoulder muscles and enhancing joint stability.
Pain management: Techniques and medications help control discomfort during recovery.
Gradual activity reintroduction: Daily tasks and functional movements are reintroduced progressively to ensure safe and effective use of the shoulder.
Following the rehabilitation plan closely ensures better outcomes, reduces the risk of re-injury, and helps patients return to their normal activities safely.
Rotator cuff injuries can often be prevented with a combination of strengthening, posture awareness, and healthy habits. Here are key strategies:
Exercise regularly: Strengthen the rotator cuff muscles and stretch the chest and back of the shoulder joint. This improves stability and reduces the risk of injury.
Maintain good posture: Poor posture can strain your shoulders. Sit upright and use lumbar support when needed.
Avoid repetitive overhead movements: Overuse can weaken the rotator cuff over time. Take breaks or modify activities to reduce strain.
Take care of overall health: Maintain a healthy weight, eat a balanced diet, stay hydrated, get adequate sleep, and avoid smoking.
Listen to your body: Seek medical advice if you experience shoulder or upper back pain to prevent worsening or future injuries.
These preventive measures help maintain shoulder strength, flexibility, and long-term joint health.
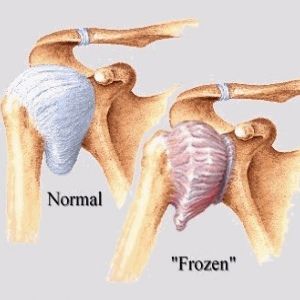
Frozen shoulder, also known as adhesive capsulitis, leads to pain, stiffness, and reduced mobility in the shoulder joint. Symptoms usually worsen gradually and then improve over time, though complete recovery may take up to three years. Physical therapy—focused on restoring shoulder flexibility—is the primary treatment to relieve discomfort and regain motion.
Frozen shoulder most often affects people between the ages of 40 and 60 and is more common in women than men. Individuals with diabetes or thyroid disorders have a higher risk, though the condition can affect anyone. In some cases, it may develop after an injury or surgery.
About Arthroscopy for Frozen Shoulder
 Symptoms
Symptoms
 Diagnosis
Diagnosis
 Why Is Treatment Needed?
Why Is Treatment Needed?
 Recovery
Recovery
 Prevention
Prevention
Frozen shoulder usually develops gradually and progresses through three stages:
Freezing Stage (2–9 months): Shoulder movements cause significant pain, and mobility becomes increasingly limited.
Frozen Stage (4–12 months): Pain may reduce, but stiffness worsens, making shoulder use more difficult.
Thawing Stage (5–24 months): Shoulder mobility begins to improve gradually, with function slowly returning.
Diagnosis of Frozen Shoulder
Physical Exam: The doctor examines the shoulder and arm, checking range of motion.
Medical History: The doctor reviews medical history and asks about symptoms.
Imaging Tests: MRI, CT scan, X-ray, or ultrasound may be used to confirm diagnosis.
MRI shows thickening of the joint capsule.
Ultrasound shows thickening of the inferior capsule, coracohumeral ligament, rotator interval changes, and restricted motion.
Frozen Shoulder (Adhesive Capsulitis)
Frozen shoulder, or adhesive capsulitis, is a condition that leads to pain and stiffness in the shoulder joint. Treatment is important to reduce discomfort, restore mobility, and preserve range of motion. Without proper care, frozen shoulder may result in long-term pain, persistent stiffness, and significant loss of shoulder function.
Recovery After Frozen Shoulder Surgery
After surgery, physical therapy is essential to maintain the motion gained during the procedure. Recovery usually takes 6 weeks to 3 months. Long-term outcomes are generally positive, with most patients experiencing little to no pain and improved mobility. However, in some cases, shoulder motion may not fully return, and mild stiffness can persist. Though uncommon, frozen shoulder can recur, especially in patients with underlying conditions such as diabetes.
One of the most common causes of frozen shoulder is limited movement of the shoulder during recovery from an injury, fracture, or stroke. If you’ve had an injury that restricts shoulder motion, consult your healthcare provider about exercises to help maintain joint mobility.
Why Choose Dr. Apoorv Dua
At our clinic, Dr. Rakesh Kumar offers specialized care for frozen shoulder. With extensive experience in orthopedic surgery, he focuses on minimally invasive techniques that promote quicker recovery and better long-term outcomes.
Patients Experience
Procedures
Trauma surgeries
Joint Replacement Surgeries
We believe in transparency. You can enquire about the Surgery Cost and we will help you with complete detailed treatment process till your recovery.
Shoulder replacement surgery is a procedure where the damaged parts of the shoulder joint are replaced with artificial implants. It is usually done to relieve severe pain, improve movement, and restore daily function when other treatments no longer work.
👉 In simple terms: It helps you get rid of constant shoulder pain and move your arm more freely.
Shoulder replacement surgery is generally very successful.
✅ Around 90–95% of patients experience significant pain relief
✅ Most regain better shoulder strength and movement
✅ Implants can last 15–20 years or more with proper care
In short: It’s a safe and effective surgery that helps most people get back to normal activities with much less pain.
Recovery from shoulder replacement surgery usually takes a few months and happens in stages:
Hospital stay: 1–3 days (some patients go home the next day).
Basic use of arm: Within 2–6 weeks (for light daily activities).
Physical therapy: Starts soon after surgery and continues for several months.
Return to normal activities: Most people regain good function in 3–6 months.
Full recovery & strength: Can take up to 12 months.
👉 Recovery speed depends on age, overall health, and how well you follow physical therapy.
The rotator cuff is a group of four muscles and their tendons that surround the shoulder joint.
Keeps the shoulder stable by holding the head of the upper arm bone (humerus) firmly in the shoulder socket.
Allows movement like lifting, rotating, and reaching with your arm.
Provides strength for overhead activities such as throwing, swimming, or painting.
the rotator cuff acts like the shoulder’s stabilizer and mover, helping you use your arm smoothly in different directions.
Surgical repair options for a rotator cuff tear usually include three main approaches, depending on the size and location of the tear:
Minimally invasive
Uses a tiny camera and small instruments through small cuts
Less pain, faster recovery
Larger incision over the shoulder
Tendon is reattached directly to the bone
Often used for big or complex tears
Combines both techniques
Surgeon uses arthroscopy first to see and clean the joint, then makes a small incision to repair the tendon
The choice depends on the size of the tear, patient’s age, activity level, and surgeon’s expertise.
Frozen shoulder is a condition where the shoulder becomes stiff, painful, and hard to move. It happens when the lining of the shoulder joint (the capsule) becomes inflamed, swollen, and tight, limiting movement.
You will likely have less pain and be able to move and use your shoulder more easily.
How to Prepare for the Operation
Stop smoking – quitting helps reduce complications and improves long-term health.
Maintain a healthy weight – being overweight can increase surgery risks.
Exercise regularly – this strengthens your body, supports recovery, and boosts overall health (ask your doctor for safe exercises).
Stay up to date with vaccinations – this lowers your risk of infection after surgery.
Follow hospital guidelines – practise good hand hygiene and wear a mask if asked.











Healing Joints and Restoring Lives with 17+ Years of Advanced Orthopedic Experience and Dedicated Patient Care
Dr. Rakesh Kumar Clinic © 2025 | Designed by ArtistryMedia